Nhân một trường hợp ống mật chủ đôi
18/12/2019 14:40:53 | 0 binh luận
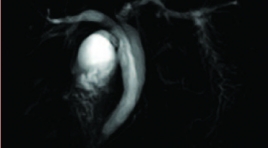
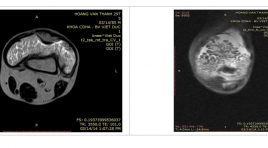
Double common bile duct: report of a case SUMMARY Double common bile duct is a rare congenital anomaly, charactered by two common bile ducts exist. One, named major common bile duct normally opens into the papilla duodeni major and the other named accessory common bile duct (ACBD) opens in different parts of upper gastrointestinal tract (stomach, duodenum, ductus pancreaticus. This anomaly is usually associated with some complications such as biliary inflammation, biliary lithiasis, choledochal cyst, anomalous pancreaticobiliary junction (APBJ), cholangiocarcinoma and upper gastrointestinal tract malignancies. We reported a 74 - year-old woman, presented with epigastric pain, chills, high fever and jaundice. Abdominal ultrasonography showed duplicated common bile duct and magnetic resonance imaging inlustrated double common bile duct type Va, classificated by Choi et al. The patient was diagnosed biliary infection without biliary lithiasis and cholangiocarcinoma, and treated with observal treatment and antibiotics. Keywords: Double common bile duct, Accessory common bile duct.
sinh thiết, chọc tế nào khối tụy và quanh tụy
17/03/2020 11:18:58 | 0 binh luận
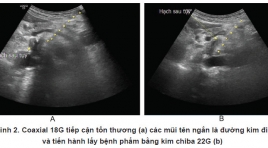
Ultrasound-guided fine needle aspiration and core needle biopsy for pancreatic neoplasms and surrounding-pancreatic neoplasms SUMMARY Solid pancreatic or peripancreatic lesions are common diseases . All most of them need to pathology diagnosis. provides an alternative pathway for adequate specimen acquisition. Because of the deep retroperitoneal location, we usually use endoscopic ultrasound (EUS)-guided fine needle aspiration (FNA) or inderect percutaneous core needle biopsy (CNB) . Both of them have disadvantages on their own. the sensitivity and specificity of EUS-guided FNA (EUS-FNA) for pancreatic neoplasms has were 85% and 98%, respectively and The complication rate of EUS-FNA is approximately 1%–2% [1]. However, one limitation related to this technique is that it often only provides a cytologic specimen with scant cellularity and lack of histologic architecture, which restrains us from making a complete tissue analysis for diagnosis and grade differentiation. the sensitivity and specificity of inderect percutaneous CNB for pancreatic neoplasms has were 90,4% and 92% respectively [2], overcome the disadvantages of EUS-FNA [3]. But it is relatively risky and difficult especially for those who do not have much experience. Reaching through the liver, spleen and kidneys increases the risk of bleeding. Approaching through the stomach and intestine, the incidence of complications can reach 15.3% [4], [5] including: infection, peritonitis and gastrointestinal perforation. Access through the gallbladder has a high risk of cholestatic and cholecystitis [4]. Derect percutaneous CNB/ FNA is a new technique which can make good the risks of two technique before. In this review, we will present some cases of FNA and biopsy of solid pancreatic or peripancreatic lesions by direct access approach, thereby showing about techniques, diagnostic effectiveness as well as complications of percutaneous CNB/ FNA. Key word: Fine needle aspiration (FNA), Core needle biopsy (CNB), Pancreas.
can thiệp nội mạch kết hợp phẫu thuận điều trị dị dạng thông động tĩnh mạch dưới da đầu phức tạp: Báo cáo trường hợp lâm sàng tại bệnh viện Việt Đức
17/03/2020 11:06:36 | 0 binh luận
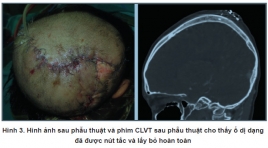
Preoperative endovascular embolisation for treatment of complicated scalp arteriovenous malformations: a case report from viet duc university hospital SUMMARY Introduction : Scalp arteriovenous malformations (sAVMs) are rare and complex vascular lesions, thought to be present at birth and characterized by variable growth leading to disfiguring and life-threatening complications. Of all vascular malformations, AVMs can be the most dangerous and difficult to manage because of their high flow, bleeding risk, and infiltrative nature. Treatment of these lesions is until a major challenge, especially for diffuse lesions, requires expert multimodal and multi-disciplinary care. Clinical case: A 12 - year - old girl, detected and partially treated for a scalp AVM of left parietal, came to the hospital because of severe bleeding from rupture sAVM. On CTA and DSA demonstrated a diffuse scalp AVM located in the parietal region, supplied from many branches of bilateral internal maxillary arteries, middle meningeal arteries, superficial temporal arteries, occipital arteries anterior cerebral artery (ACA), drainage to superior sagittal sinus. The sAVM’s feeders were catheterized and totally embolized by combine through transfemoral artery, transfemoral vein, and direct percutaneous approach. Surgical resection the nidus was performed 4 days after. Conclusion : The complex scalp AVM lesions are always major challenges in treatment. Endovascular embolization plays an important role in reducing complications and increasing the ability to completely remove lesions. Keywords : Scalp arteriovenous malformations, endovascular embolization.

Phình khổng lồ tiểu nhĩ trái: báo cáo một trường hợp hiếm gặp tại bệnh viện Bạch Mai
30/03/2020 15:35:19 | 0 binh luận
Giant left atrial appendage aneurysm with radiology: case report and literature SUMMARY We report a extremely rare case of 16-year-old boy with a giant left atrial appendage aneurysm. Patient‘s symptoms are dyspnea and atrial tachyarrhythmia. The exact diagnosis is make by chest X-ray, echocardiography (transthoracic and transoesophageal), magnetic resonance imaging, and multislice computer tomographic angiography. The patient was successfully treated with surgical resection of the aneurysm. For its rarity, this case is reported and review about literature of aneurysm of left atrial appendage. Because of dangerous of atrial aneurysm (dangerous fifth chamber cardiac) with supraventricular arrhythmias and systemic thromboembolism, surgical resection is the best method to avoid further complication and recurrence. Key word : Giant left atrial aneurysm.
Nghiên cứu kết quả ban đầu sử dụng hạt vi cầu embozene trong diều trị nút mạch u cơ trơn tử cung
30/03/2020 14:21:25 | 0 binh luận
The initial effect of embolization of uterine leiomyomas with embozene spheres SUMMARY Purpose Evaluating the initial effect of fibroid embolization procedure with embozene microspheres at Bach Mai radiology department. Methods and objectives Follow - up study from January 2015 to February 2016, we treated 41 patients who manifest symptom clinically (mean ± SD age 37.3 ± 5.7 years, range 24-47 years). Assessing including: clinical symptom, volume of fibroid after treatment 1 month, 3 months, 6 months by ultrasound and magenic resonance imaging after 6 months. Results The mean tumor volume 65.6 ± 5. 8 ml (range 1.7-353). A total of 51 tumors of 41 patients were carried out intervention, a technical success rate of 100%. Post intervention 54% patients were painless, the mean pain time 1.2 ± 0.7 day. There are no main complication. After 6 months, 96.1% patients stopped hypermenorrhea, 94.4% patients disappeared abdominal pain. Quality of life index improved 3.8 point. The tumor volume decrease 19.6% after 1 month, 53.3% after 3 months, 80.1% after 6 months (P < 0.001). Conclusion Embozene microspheres is a potentially chosen material inuterine artery embolization because of its safe and effective procedure. Key words : fibroid, uterine artery embolization, embozene microspheres.
Nhân một trường hợp đa u mỡ bao hoạt dịch khớp gối được chẩn đoán bằng cộng hưởng từ
23/05/2020 11:33:48 | 0 binh luận
Synovial Lipomatosis (Lipoma arborescens) of the knees - case report SUMMARY Synovial Lipomatosis is a rare benign that can present with monoarticular or polyarticular involvement of joints such as knees, ankles, hips, shoulders, and elbows [5]. We describe a case in a 29-year-old man who presented with prolonged pain and swelling of the bilateral knee joints for the previous 20 years. Plain radiograph usually shows joint fullness and osteoarthritic changes. MRI show a thickening of the synovium that has the characteristic features of fat and joint effusion of the bilateral knee joints. Therefore, the patient was underwent synovectomy, which revealed a diffuse yellow soft tissue synovial papillary growth from synovial pouch. The pathology was synovial lipomatosis. This is the first case of Viet Duc Hospital. It is also termed as villous lipomatous proliferation of the synovium or lipoma arborescens, diffuse lipoma of the joint, diffuse synovial lipoma, diffuse articular lipomatosis, fatty infiltration of the synovial membrane, villous lipomatous proliferation of the synovial membrane [8]. Key words: Synovial Lipomatosis, knees.
Nhân hai trường hợp Schizencephaly
31/03/2020 22:28:11 | 0 binh luận
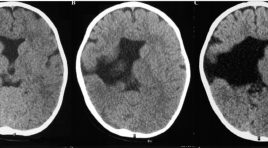
Schizencephaly – 2 cases report SUMMARY Introduction: Schizencephaly is a congentital brain malformation, which is characterized by clefts extending from pial surface of cerebral mantle to ventricle. This morphologically malformation divides into 2 types “closed-lip” and “open-lip”. Clinical symptoms ranged from simple to complicated depend on the location of clefts. This is a rare malformation, according to statistics, the incidence of the disease is approximately 1-2: 100.000 populations. Therefore, we are describing 2 cases encountered in Hue UniversityHospital within 2 years. Approach :Case 1: 2-year-old male patient, presenting the clinical symptom of half body weakness since 8 months old. Pregnant history of his mother were been unexplained fever in 8th month pregnancy, untreated. He underwent brain CT scanner and MRI. Case 2: 33-year-old male, hospitalization by presenting the epilepsy. He has been the half body weakness since neonatal phase. He underwent brain MRI. Result : Case 1: Presenting a large cleft lined by grey matter between right ventricle and pial surface of right hemisphere. Right parietal, temporal, and frontal lobeswere atrophic; the septum pellucidum is absent. Posterior part of corpus callosum was atrophic Case 2: Large size cleft lined by grey matter between right ventricle and pial surface of right hemisphere. Right frontal lobe is small. Right frontal gyri and lined-cleft gyri are small, hyperdensity. Medial line deviates toward left side. Corpus callosum is normal. Conclusion : Schizencephaly malformation occurs in any ages with different clinical symptoms. Typical character is the cleft, which is lined by grey matter from ventricle to arachinoid space. This accompanies other abnormalities such as the absence of septum pellucidum, polygyri, atrophy of corpus callosum. Diagnostic imaging, especially MRI, is crucially important to define this malformation and accompied abnormalities. Key words: Schizencephaly, MRI.
Đánh giá tính an toàn và hiệu quả nút mạch phối hợp bơm trực tiếp ổ dị dạng thông động tĩnh mạch vùng đầu mặt cổ trước phẩu thuật
02/04/2020 22:20:34 | 0 binh luận
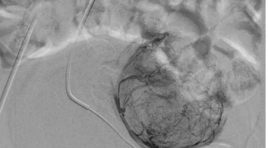
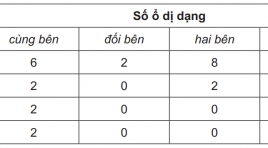
Evaluate the safety and effectiveness of ercutaneous direct puncture glue embolization accompanying with endovascular embolization of cervicofacial arteriovenous malformation prior to extirpation SUMMARY: Objects: Evaluate the safety and effectiveness of percutaneous direct puncture glue embolization accompanying with endovascular embolization of cervicofacial arteriovenous malformation prior to extirpation. Subjects and method: Clinical trial without control, achieved in 16 patients in a period from August 2008 to April 2012 at Vietduc Friendship Hospital. Results: 16 patients was carried out endovascular for facial AVM embolization accompanying percutaneous direct puncture embolization, mostly in the age of 20 to 40 (66.5%). There are 20 times of pre-operative embolization, achieving 80% almost occlusion (>80%), extirpation in 94% of cases, hemostatic effect achieved in 88.2%. The length of hospital stay of patients who had one time of embolization and extirpation is 11,9 days. Conclusion: Percutaneous direct puncture accompanying with endovascular glue embolization is a safe and effective procedure, which reduces surgical bleeding and achieves the ability of total extirpation, avoids recurrence. Keyword: arterovenous malformation, endovascular embolization, percutaneous direct puncture, glue.
Bạn Đọc Quan tâm
Sự kiện sắp diễn ra
Thông tin đào tạo
- Những cạm bẫy trong CĐHA vú và vai trò của trí tuệ nhân tạo
- Hội thảo trực tuyến "Cắt lớp vi tính đếm Photon: từ lý thuyết tới thực tiễn lâm sàng”
- CHƯƠNG TRÌNH ĐÀO TẠO LIÊN TỤC VỀ HÌNH ẢNH HỌC THẦN KINH: BÀI 3: U não trong trục
- Danh sách học viên đạt chứng chỉ CME khóa học "Cập nhật RSNA 2021: Công nghệ mới trong Kỷ nguyên mới"
- Danh sách học viên đạt chứng chỉ CME khóa học "Đánh giá chức năng thất phải trên siêu âm đánh dấu mô cơ tim"