MÔ TẢ ĐẶC ĐIỂM HÌNH ẢNH DI CĂN GAN Ở BỆNH NHÂN UNG THƯ ĐẠI TRỰC TRÀNG TRÊN CLVTV
17/10/2023 17:47:51 | 0 binh luận
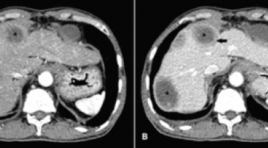
SUMMARY Background: Colorectal cancer is a common cancer that has a high morbidity and mortality rate, and the liver is the most frequent metastatic organ. Dynamic computed tomography (CT) can be used to diagnose colorectal liver metastases based on their imaging characteristics and enhancing patterns which are different from other liver lesions. Objective: To describe the imaging characteristics of colorectal liver metastases on dynamic CT. Methods: A cross–sectional study was conducted on 39 colorectal cancer patients with pathologically proven liver metastases. All patients underwent triphasic CT. Other lesions sharing similar imaging characteristics were considered metastases. Patient demographic and CT findings were documented Results : 39 patients and 92 lesions were included in the analysis. Liver metastases can be solitary (48.7%) or multiple (51.3%). Most of them are located in the right lobe (62%) more than the left lobe. Lesions less than 5 cm have the highest rate (80.5%). Liver metastases are often well–defined (54.4%) with non-lobulated borders (58.7%). Calcification is rare (5.4%). Compared to the surrounding liver parenchyma, colorectal liver metastases have a lower density in the pre-contrast phase (89.3%), and are also less enhanced in arterial and venous phases (93.5% and 98.9% gradually). Contrast-enhanced lesions are usually heterogeneously (91.3%). Rim enhancement at the peripheral area is often observed (78.2%). Of 51 lesions, it appears on both arterial and venous phases (55.4%). Central necrosis is about 41.3% of the total lesions and dominantly appears in lesions larger than 3 cm. Conclusions: Imaging characteristics of the colorectal liver metastases mostly observed are the thin rim enhancement at the peripheral area, low density in the pre-contrast phase, less enhancement than the normal surrounding liver parenchyma on both arterial and venous phases, central necrosis in the large lesions, and heterogeneously enhanced pattern. Keywords : colorectal liver metastases, dynamic CT, imaging characteristics.
BÁO CÁO CA LÂM SÀNG: TĂNG SẢN THỂ NỐT KHU TRÚ GAN SAU HÓA CHẤT ĐIỀU TRỊ UNG THƯ DẠ DÀY
17/10/2023 16:10:46 | 0 binh luận
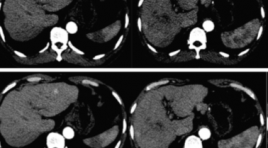
SUMMARY Chemotherapy could induce multiple liver parenchymal and vascular disorder presenting as diffuse or focal lesion. Focal nodular hyperplasia (FNH) – like nodules is benign lesions that should be distinguish to hepatic metastasis because they associate with further interventions and treatments. The main machanism of the apperance of FNH is Oxaliplatin-induced portal venous injuries called hepatic sinusoid obstruction syndrome (HSOS). Here, we present a case of the development of FNH – like nodule during follow up of gastric carcinoma after adjuvant treatment with XELOC chemotherapy (Oxaliplatin-based chemotherapy). Keywords: focal nodular hyperplasia like nodule, hepatic sinusoid obstruction syndrome, chemotherapy - induced liver injury
SARCOMA MẠCH MÁU NGUYÊN PHÁT TẠI GAN: THÔNG BÁO CA LÂM SÀNG
17/10/2023 15:59:04 | 0 binh luận
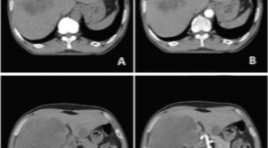
SUMMARY We report a case who was diagnosed with primary hepatic angiosarcoma (PHA). A 62-year-old man presented with right upper quadrant abdominal pain, weight loss, and hepatomegaly. He did not have a history of carcinogen exposure or any relevant medical history. On laboratory evaluation, the patient had an elevation of white blood cell count, AST, ALT and anemia. The levels of serum carcinoembryonic antigen, carbohydrate antigen (CA)-19-9, α-fetoprotein, and PIVKA-II were normal. Abdominal ultrasound, computed tomography, and magnetic resonance imaging revealed a large lesion in the right lobe of the liver and a small lesion in the left lobe of the liver which are non-specific images. The patient underwent liver biopsy and histopathological examination confirmed PHA. PHA is a rare disease that usually occurs in the sixth decade of life, and males are more frequently affected than females. In most cases, the cause is unknown. Clinical symptoms and laboratory evaluation of PHA are nonspecific. There is no pattern recognition in diagnostic imaging. Liver biopsy and histopathology confirmed the presence of PHA. Keywords : angiosarcoma, primary hepatic angiosarcoma.
THOÁT VỊ NỘI SAU MỔ CẮT ĐOẠN DẠ DÀY: BÁO CÁO 2 TRƯỜNG HỢP VÀ TỔNG QUAN Y VĂN
17/10/2023 15:54:43 | 0 binh luận
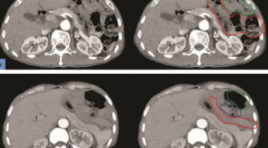
SUMMARY Objective: Internal hernia following gastrectomy is an uncommon disease. Preoperative diagnosis is difficult because clinical symptoms are nonspecific. However, it is a surgical emergency, accurate preoperative diagnosis is crucial for appropriate management. Multidetector computed tomography (CT) plays an essential role in preoperative diagnosis of internal hernias. Methods: Describing 2 cases, at Thong Nhat Hospital, Ho Chi Minh City. All patients went preoperative CT and proved surgically internal hernias: Peterson hernia, J-J hernia. Results: The combination of mesenteric swirl sign and small bowel obstructioon has the highest sensitivity and accuracy for internal hernia following gastrectomy. “Sandwich sign” an interposed small bowel between transverse colon and gastrojejunostomy’s limb can be a predictor of Peterson hernia. Meanwhile, the positon of hernia orifice, which is close to the position of J-J anastomosis and the displacement of J-J anastomosis out of the left-mid abdomen can predict J-J hernia. Conclusions: Multidetector computed tomography (CT) plays an essential role in preoperative diagnosis of internal hernias following gastrectomy. Keywords: internal hernia, gastrectomy, multidetector computed tomography, Peterson hernia, J-J hernia.
GIÁ TRỊ CỘNG HƯỞNG TỪ XÓA NỀN 3.0 TESLA ĐÁNH GIÁ TĂNG SINH MẠCH Ở BỆNH NHÂN UNG THƯ BIỂU MÔ TẾ BÀO GAN SAU TACE
17/10/2023 11:01:54 | 0 binh luận
SUMMARY Objective: The value of dynamic subtraction MRI 3.0 Tesla technique in the angiogenesis assessment of hepatocellular carcinoma after transcatheter arterial chemoembolization. Methods: A cross-sectional, retrospective descriptive study was performed on 40 patients, who had been diagnosed with HCC and treated with TACE, then do dynamic subtraction MRI 3T from 6/2021 to 6/2022 at Bach Mai hospital, Hanoi, Vietnam. Result: The study consisted of 40 patients with 57 hepatocellular carcinoma lesions who underwent transarterial chemoembolization procedure and followed up by dynamic MRI of the liver with post processing to obtain subtraction images and compared with DSA. The subtraction images have sensitivity of 100%, specificity of 100%, PPV of 100%, and NPV of 100%. On the other hand, the dynamic images is 90,9%; 69,2%; 90,9%;69,2%; the Diffusion images is 97,7%; 61,5%; 89,6%; 88,9%. Comparative study between D-MRI and DS-MRI assessments revealed; highly significant increase in disease detection rate, sensitivity, and NPV in favor of DS-MRI in HCC patients; with highly significant difference (p < 0.01 respectively). Conclusions: Dynamic MRI is valuable in the angiogenesis assessment of hepatocellular carcinoma after TACE, however, this value is augmented by the addition of subtraction technique especially in lesions having high signal before administration of contrast medium with sensitivity of 100%, specificity of 100%, PPV of 100%, and NPV of 100%. So we recommend adding the subtraction technique in the protocol of MRI in the follow up after transarterial chemoembolization as it increases the diagnostic confidence. Keywords: dynamic subtraction MRI, hepatocellular carcinoma, TACE.
VAI TRÒ CỦA CỘNG HƯỞNG TỪ TRONG CHẨN ĐOÁN U TUYẾN THƯỢNG THẬN
11/10/2023 15:01:16 | 0 binh luận
SAMMARY Purpose: to evaluate the role of MRI in diagnosis adrenal tumors. Subject and methods: our cross–sectional descriptive study included 25 patients who were diagnosed as adenoma hyperplasia in pathology. All patients underwent MRI examination in Bach Mai hospital from June, 2020 to July, 2021. Results: mean age of all patient was 49,2±11,8. Male/female ratio was 1.5/1. 25 adrenal tumor on MRI and identified on the diagnosed as adenoma hyperplasia in pathology. These adenomas consisted 12 adrenal cortical adenoma (ACA) and 13 non – adrenal cortical adenoma (NACA): 09 pheochromocytomas, 01 adrenocortical carcinoma, 01 ganglioneuroma and 02 myelolipoma. Mean size of all adrenal tumors was 38,8 ± 23,5mm, therein, mean size of ACA group and NACA group was 23,2 ± 7,6 mm and 52,2 ± 25,7 mm respectively. Chemical Shift Imaging (CSI) allowed differential diagnose between ACA and NACA. Qualitative analysis based on signal reduction on out – phase compared to in – phase allows 11/12 ACA, but 2/13 NACA have been misdiagnosed as ACA. Quantitative analysis based on SII index (SII threshold > 16,1%) allowed correctly diagnose 11/12 ACA and 01 NACA. ASR index (ASR threshold <0,71) allowed correctly diagnose 11/12 ACA and 01 NACA. There are 02 adrenal tumors that invaded to the surrounding area in imaging and was demonstrated by surgery and pathology reports. Conclusion : MRI has an important role in adrenal mass diagnosis with sensitivity and specificity were 100% and 96,1% respectively. CSI enable to distinguish ACA and NACA with sensitivity and specificity were 91,7% and 92,3% respectively by using SII and ASR index. MRI also help to assess invasive and metastatic properties with high accuracy. Key words : adrenal tumors, adrenal MRI, chemical shift imaging (CSI).

ĐÁNH GIÁ HIỆU QUẢ ĐIỀU TRỊ UNG THƯ BIỂU MÔ TẾ BÀO GAN BẰNG NÚT MẠCH VI CẦU PHÓNG XẠ YTTRIUM-90
11/10/2023 14:52:30 | 0 binh luận
SUMMARY Background: Hepatocellular carcinoma (HCC) is the second most common cause of cancer-related deaths worldwide. Radioembolization with Yttrium-90 is a safe, effective locoregional therapy for unresectable HCC. Purpose: This study aimed to evaluate the safety and efficacy of radioembolization with Yttrium-90 for the treatment of HCC. Materials and methods: A total of 93 patients were diagnosed with HCC and treated by radioembolization with Yttrium-90 from 2013 to 2021 at Bach Mai Hospital. Radiographic findings on computed tomography (CT) or magnetic resonance imaging (MRI) were assessed by using modified Response Evaluation Criteria in Solid Tumors (mRECIST). Patient survival was assessed using the Kaplan-Meier method, and prognostic factors affecting survival were assessed using Cox proportional hazards regression. Results: The mean age of 93 patients was 59.0±9.8 years. Mean tumors diameter was 6.5 ± 2.7 cm, the mean of tumor marker AFP is 1812 ± 6577 ng/ml. Complete response and partial response to treatment were observed in 21 (40.4%) and 15 patients (28.8%) of 52 follow-up patients. The median overall survival (OS) was 12.0 [95% CI: 5.0-25.0] months. Factors associated with longer OS included BCLC stage A-B, ECOG 0 and no portal vein thrombosis. Conclusion: Radioembolization with Y-90 is safe and effective in patients with unresectable HCC. BCLC stage A-B, ECOG 0 and no portal vein thrombosis were positive prognostic factors. Keywords: Hepatocellular carcinoma, radioembolization, Selective internal radiation therapy, Yttrium-90, Tumor response
ĐẶC ĐIỂM HÌNH ẢNH CHT 4 CA TEO ĐƯỜNG MẬT BẨM SINH THỂ CÓ NANG GIỐNG U NANG ỐNG MẬT CHỦ
11/10/2023 14:44:26 | 0 binh luận
SUMMARY Purpose: to describle in detail the significant signs in hepatobiliary MRI, that help to give different diagnosis between biliary atresia (BA) with big cyst at hepatic hilar and choledochal cyst in small childrent and infant. Method: presenting 4 cases with clinical diagnosed of biliary atresia that based on clinical signs and US, MRI results, all 4 cases were operated, taken cholangiogram in surgery to confirm the diagnosis of cystic biliary atresia and had pathological results. Results: All 4 patients were under 3 months old, all are female with enlarged liver; gallbladder were in the normal size limit but all of them had abnormal shape: deformation, irregular wall, communicated directly with common bile duct. All 4 cases have cystic diameter over 10mm. No case of all has further biliary signal that above or under the cyst on MRI but one case has contrast material filling intraliver bile duct draining directly to cystic lesion on cholangiogram intraoperation . These are 3 cases of cystic BA type III and 1 cases of cystic BA type I. 2 cases has positive triangular cord sign (TC sign). Conclusion : Hepatobiliary MRI with its basic sequences, specially with MRCP is helpful to give difirential diagnosis of cystic BA and choledochal cyst in the young childrent. Keyword: Biliary atresia, cystic biliary atresia
Bạn Đọc Quan tâm
Sự kiện sắp diễn ra
Thông tin đào tạo
- Những cạm bẫy trong CĐHA vú và vai trò của trí tuệ nhân tạo
- Hội thảo trực tuyến "Cắt lớp vi tính đếm Photon: từ lý thuyết tới thực tiễn lâm sàng”
- CHƯƠNG TRÌNH ĐÀO TẠO LIÊN TỤC VỀ HÌNH ẢNH HỌC THẦN KINH: BÀI 3: U não trong trục
- Danh sách học viên đạt chứng chỉ CME khóa học "Cập nhật RSNA 2021: Công nghệ mới trong Kỷ nguyên mới"
- Danh sách học viên đạt chứng chỉ CME khóa học "Đánh giá chức năng thất phải trên siêu âm đánh dấu mô cơ tim"