MÔ TẢ ĐẶC ĐIỂM HÌNH ẢNH DI CĂN GAN Ở BỆNH NHÂN UNG THƯ ĐẠI TRỰC TRÀNG TRÊN CLVTV
17/10/2023 17:47:51 | 0 binh luận
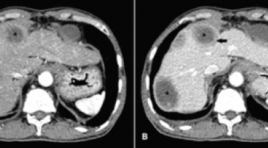
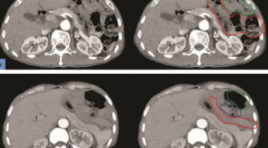
SUMMARY Background: Colorectal cancer is a common cancer that has a high morbidity and mortality rate, and the liver is the most frequent metastatic organ. Dynamic computed tomography (CT) can be used to diagnose colorectal liver metastases based on their imaging characteristics and enhancing patterns which are different from other liver lesions. Objective: To describe the imaging characteristics of colorectal liver metastases on dynamic CT. Methods: A cross–sectional study was conducted on 39 colorectal cancer patients with pathologically proven liver metastases. All patients underwent triphasic CT. Other lesions sharing similar imaging characteristics were considered metastases. Patient demographic and CT findings were documented Results : 39 patients and 92 lesions were included in the analysis. Liver metastases can be solitary (48.7%) or multiple (51.3%). Most of them are located in the right lobe (62%) more than the left lobe. Lesions less than 5 cm have the highest rate (80.5%). Liver metastases are often well–defined (54.4%) with non-lobulated borders (58.7%). Calcification is rare (5.4%). Compared to the surrounding liver parenchyma, colorectal liver metastases have a lower density in the pre-contrast phase (89.3%), and are also less enhanced in arterial and venous phases (93.5% and 98.9% gradually). Contrast-enhanced lesions are usually heterogeneously (91.3%). Rim enhancement at the peripheral area is often observed (78.2%). Of 51 lesions, it appears on both arterial and venous phases (55.4%). Central necrosis is about 41.3% of the total lesions and dominantly appears in lesions larger than 3 cm. Conclusions: Imaging characteristics of the colorectal liver metastases mostly observed are the thin rim enhancement at the peripheral area, low density in the pre-contrast phase, less enhancement than the normal surrounding liver parenchyma on both arterial and venous phases, central necrosis in the large lesions, and heterogeneously enhanced pattern. Keywords : colorectal liver metastases, dynamic CT, imaging characteristics.
CAN THIỆP NỘI MẠCH HUYẾT KHỐI TĨNH MẠCH SÂU CHI DƯỚI
17/10/2023 17:23:19 | 0 binh luận
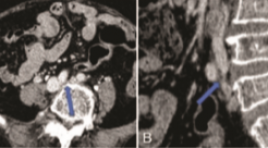
SUMMARY Endovascular management of the lower extremity deep vein thrombosis Lê Trọng Bỉnh Lower extremity deep vein thrombosis (LEDVT) is a common vascular disease which may cause life-threatening complications such as pulmonary embolism or lead to lifelong sequelae such as post-thrombotic syndrome. Anticoagulation remains the standard treatment of LEDVT endorsed by various international practice guidelines. However, anticoagulation alone is usually inadequate in the setting of large thrombus burden (iliofemoral DVT), extensive LEDVT (inferior vena cava extension), and venous outflow obstruction (eg, May-Thurner syndrome), therefore increases the risk of delayed symptom alleviation, thrombus recurrence, and disease progression. Prompt diagnosis and timely intervention including effective thrombus exclusion and venous outflow recanalization are crucial in optimizing treatment outcomes, limiting complications, and preventing further sequelae. Recently, endovascular approach has shown advantages over open surgery and medical treatment in selected populations of LEDVT. This minimally invasive technique includes a single-session and step-by-step intervention combining an inferior vena cava filter insertion, catheter-directed thrombolysis, mechanical thrombectomy, and iliocaval recanalization by venoplasty and/or stenting. This paper aims to provide insight into the current status of endovascular treatment of LEDVT and experience from a single center. Keywords: deep vein thrombosis, thrombolysis, thrombectomy, endovascular, May-Thurner syndrome
BÁO CÁO CA LÂM SÀNG: TĂNG SẢN THỂ NỐT KHU TRÚ GAN SAU HÓA CHẤT ĐIỀU TRỊ UNG THƯ DẠ DÀY
17/10/2023 16:10:46 | 0 binh luận
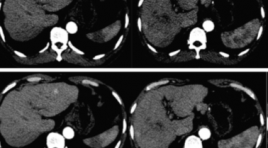
SUMMARY Chemotherapy could induce multiple liver parenchymal and vascular disorder presenting as diffuse or focal lesion. Focal nodular hyperplasia (FNH) – like nodules is benign lesions that should be distinguish to hepatic metastasis because they associate with further interventions and treatments. The main machanism of the apperance of FNH is Oxaliplatin-induced portal venous injuries called hepatic sinusoid obstruction syndrome (HSOS). Here, we present a case of the development of FNH – like nodule during follow up of gastric carcinoma after adjuvant treatment with XELOC chemotherapy (Oxaliplatin-based chemotherapy). Keywords: focal nodular hyperplasia like nodule, hepatic sinusoid obstruction syndrome, chemotherapy - induced liver injury

UNG THƯ PHỔI DI CĂN ĐẠI TRÀNG: BÁO CÁO CA BỆNH VÀ ĐỐI CHIẾU Y VĂN
17/10/2023 16:02:52 | 0 binh luận
SUMMARY Lung cancer is one of the leading causes of cancer related mortality worldwide. The brain, liver, adrenal glands, and bone are the most likely site of metastatic disease in patients with lung cancer. Gastrointestinal (GI) metastasis from primary lung cancer is very rare. Only few reports have been published and the majority of described metastatic sites involved the small instestine. In the present study, we report a case of lung cancer with colonic metastasis and also review the published literature of primary lung cancer with colonic metastasis. Keywords : lung cancer, gastrointestinal metastasis, colonic metastasis.
SARCOMA MẠCH MÁU NGUYÊN PHÁT TẠI GAN: THÔNG BÁO CA LÂM SÀNG
17/10/2023 15:59:04 | 0 binh luận
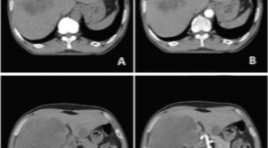
SUMMARY We report a case who was diagnosed with primary hepatic angiosarcoma (PHA). A 62-year-old man presented with right upper quadrant abdominal pain, weight loss, and hepatomegaly. He did not have a history of carcinogen exposure or any relevant medical history. On laboratory evaluation, the patient had an elevation of white blood cell count, AST, ALT and anemia. The levels of serum carcinoembryonic antigen, carbohydrate antigen (CA)-19-9, α-fetoprotein, and PIVKA-II were normal. Abdominal ultrasound, computed tomography, and magnetic resonance imaging revealed a large lesion in the right lobe of the liver and a small lesion in the left lobe of the liver which are non-specific images. The patient underwent liver biopsy and histopathological examination confirmed PHA. PHA is a rare disease that usually occurs in the sixth decade of life, and males are more frequently affected than females. In most cases, the cause is unknown. Clinical symptoms and laboratory evaluation of PHA are nonspecific. There is no pattern recognition in diagnostic imaging. Liver biopsy and histopathology confirmed the presence of PHA. Keywords : angiosarcoma, primary hepatic angiosarcoma.
THOÁT VỊ NỘI SAU MỔ CẮT ĐOẠN DẠ DÀY: BÁO CÁO 2 TRƯỜNG HỢP VÀ TỔNG QUAN Y VĂN
17/10/2023 15:54:43 | 0 binh luận
SUMMARY Objective: Internal hernia following gastrectomy is an uncommon disease. Preoperative diagnosis is difficult because clinical symptoms are nonspecific. However, it is a surgical emergency, accurate preoperative diagnosis is crucial for appropriate management. Multidetector computed tomography (CT) plays an essential role in preoperative diagnosis of internal hernias. Methods: Describing 2 cases, at Thong Nhat Hospital, Ho Chi Minh City. All patients went preoperative CT and proved surgically internal hernias: Peterson hernia, J-J hernia. Results: The combination of mesenteric swirl sign and small bowel obstructioon has the highest sensitivity and accuracy for internal hernia following gastrectomy. “Sandwich sign” an interposed small bowel between transverse colon and gastrojejunostomy’s limb can be a predictor of Peterson hernia. Meanwhile, the positon of hernia orifice, which is close to the position of J-J anastomosis and the displacement of J-J anastomosis out of the left-mid abdomen can predict J-J hernia. Conclusions: Multidetector computed tomography (CT) plays an essential role in preoperative diagnosis of internal hernias following gastrectomy. Keywords: internal hernia, gastrectomy, multidetector computed tomography, Peterson hernia, J-J hernia.
KHẢO SÁT VỊ TRÍ LỖ THÔNG XOANG BƯỚM Ở NGƯỜI TRƯỞNG THÀNH TRÊN CẮT LỚP VI TÍNH
17/10/2023 15:27:45 | 0 binh luận
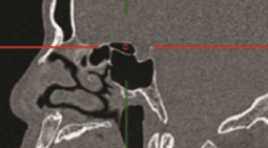
SUMMARY Background: The sphenoid sinus is closely surrounded by many important vascular and neurological. The natural ostium is the safest place to enter the sphenoid sinus without injuring adjacent structures. A better understanding of the position and distance of the sphenoid ostium (SO) with respect to the other anatomic landmark is essential for the safety and effectiveness of laparoscopic surgery. Objective: The purpose of this study was to investigate the relationship between the SO and surrounding landmark structures. Besides, we examine the effect of the Onodi cell and pneumatization of the sphenoidal sinus on the position of the SO. Methods: Cross-sectional study of 162 sinus CT scan data obtained from the PACS system at University Medical Center Ho Chi Minh City. The image is reconstructed and measured by the Multiplanar reconstruction (MPR) software of the PACS Carestream. Results: The mean distance between the SO and the lateral wall was 9.1 ± 1.8 mm. The mean distance from the SO to the median line was 4.1 ± 1.8 mm. The mean distance between the SO and the roof sphenoid sinus was 7.9 ± 2.9 mm. The average distance from the sphenoid ostium to superior border of posterior choana was 12.9 ± 3.5 mm. The mean distance from the sphenoid ostium to the anterior nasal spine was 65.2 ± 4.5 mm and to the posterior wall of the sphenoid sinus was 12.8 ± 2.7 mm. The angle between the SO - the anterior nasal spine and the floor of the nose is 33.5 ± 3.5 degrees. The distance from the SO to the roof sphenoid sinus was found to increase in cases where Onodi cells are present. For lateral pneumatization, the distance from the SO to the lateral wall in type II to be less in type III. The sphenoid sinus pneumatization on the sagittal plane did not affect the distance from SO to the posterior choana and the roof sphenoid sinus. Conclusions: The study determined the distances between the SO and some surrounding anatomical landmarks, and also investigated the influence of the Onodi cell and pneumatization on the position of the sphenoid sinus by CT scan images. The measurements described in this study may be very valuable in avoiding serious complications while performing surgery. Keywords: Sphenoid ostium, computed tomography.
ĐẶC ĐIỂM HÌNH ẢNH SIÊU ÂM, CỘNG HƯỞNG TỪ VÀ CHỤP MẠCH SỐ HOÁ XOÁ NỀN CỦA MỘT SỐ BỆNH NHÂN TĂNG SẢN LÀNH TÍNH TUYẾN TIỀN LIỆT
17/10/2023 15:05:17 | 0 binh luận
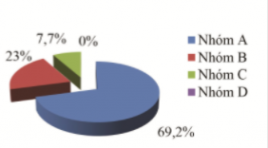
SUMMARY Objective: Describe Imaging features Ultrasound, MRI and DSA of 14 patients who have benign prostatic hyperplasia with acute urinary retention, were treated by PAE. Method and results: A descriptive study without control in patients hospitalized for acute urinary retention was diagnosed with benign prostatic hyperplasia at the Bach Mai hospital from 07/2017 to 07/2018. The patients were examined clinical, ultrasound, MRI before and after intervention. The average PV (cm3) on ultrasound and MRI are 80,57±50,58 cm3 and 82,35±51.24 cm3, 9 patients have thickening of bladder wall (64,3%), 3 patients have bladder diverticulum (21,4%), 78,6% hyperplasia at the transition zone, 7,1% hyperplasia at the central zone and 14,3% hyperplasia at both the transition zone and central zone. On DSA, with 26 pelvices side were perfomed successful, there were 22 pelvices side with one prostate artery and 4 pelvices side with 2 prostate arteries, the average diameter of prostate with pelvic side which one prostate artery is 1,92 ± 0,52 mm; with pelvic side which two prostate arteries is 1,45 ± 0,16mm. Keywords : prostatic arterial embolization, acute urinary retention, benign prostatic hyperplasia, ultrasound, MRI of BPH.
Bạn Đọc Quan tâm
Sự kiện sắp diễn ra
Thông tin đào tạo
- Những cạm bẫy trong CĐHA vú và vai trò của trí tuệ nhân tạo
- Hội thảo trực tuyến "Cắt lớp vi tính đếm Photon: từ lý thuyết tới thực tiễn lâm sàng”
- CHƯƠNG TRÌNH ĐÀO TẠO LIÊN TỤC VỀ HÌNH ẢNH HỌC THẦN KINH: BÀI 3: U não trong trục
- Danh sách học viên đạt chứng chỉ CME khóa học "Cập nhật RSNA 2021: Công nghệ mới trong Kỷ nguyên mới"
- Danh sách học viên đạt chứng chỉ CME khóa học "Đánh giá chức năng thất phải trên siêu âm đánh dấu mô cơ tim"